Mobile Integrated Healthcare Symposium

Save the Date!
Friday, October 10th | 9 am – 4 pm | Pasco, WA
Registration Coming Soon!
Greater Health Now invites you to our second annual Mobile Integrated Healthcare Symposium.
We’re excited to bring together emergency medical services (EMS), clinicians, and policy-makers to collaborate on the growing field of mobile integrated healthcare in Washington state.
This one day conference will provide an opportunity to exchange best-practices, celebrate successes, and build relationships.
Mobile Integrated Health Program
Mobile Integrated Health Program Overview
Mobile Integrated Health Program, a year after Greater Health Network (GHN introduced it, marks a significant stride in healthcare delivery. The CP program saw successful collaborations with nine regional fire departments, focusing on diminishing non-critical 911 calls and unnecessary visits to the emergency department.
Investment in community alliances has been pivotal, engendering stronger ties with local organizations, medical facilities, and service providers to ensure an efficient allocation of resources and prevent service duplication. Community Paramedicine, while not entirely novel, is experiencing a transformative expansion within our region. Notable developments include a reported 33% reduction in non-emergent EMS calls by one of the fire departments, underpinning the program’s effectiveness in communities and the healthcare system. With year two dawning, the fire departments are poised to fortify and expand their CP programs.
The goal is to reinforce their impact on patients, the wider community, and the healthcare ecosystem at large. Community Paramedics proactively engage challenges at their source, endeavoring to root out and tackle fundamental health issues. Their strategic initiatives are instrumental in enhancing patient health and curtailing the excessive use of emergency resources. The spectrum of services launched by the fire departments encompasses a comprehensive approach, ranging from health
and social needs screenings to risk and fall evaluations.
These services also extend to resource navigation—identifying providers for primary care, ensuring food security, and issuing emergency housing vouchers. Moreover, apart from facilitating transportation for patients to attend appointments, the program supports medication adherence and offers thorough discharge planning. Community paramedics also conduct home visits for safety checks like smoke alarm replacements and building ramps for accessibility. Preparing homes for a comfortable transition post-hospitalization or rehabilitation facility discharge is another facet of
these invaluable services.
Year One Outcomes
- Reduction in EMS calls across the entire cohort, 26% decrease in Upper Kittitas County!
- Increased collaborations between EMS and hospitals, behavioral health providers, community-based organizations.
- Risk stratification of high-risk, high-utilizers, allowing for proactive interventions.
- Development of Community Fall Prevention programs.
- Medication pick up, delivery and management.
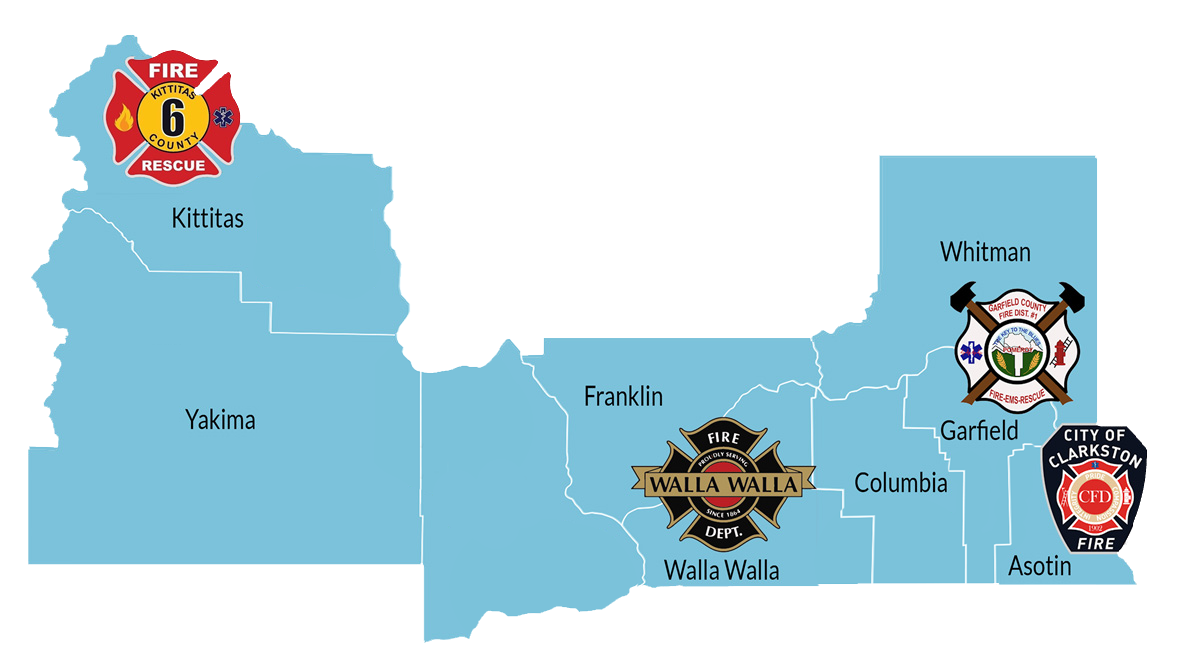
Mobile Integrated Health Program Sites
- City of Clarkston Fire Department -Asotin
- City of Walla Walla Fire and Ambulance Department
- Garfield County Fire District #1
- Kittitas County Fire Protection District 6